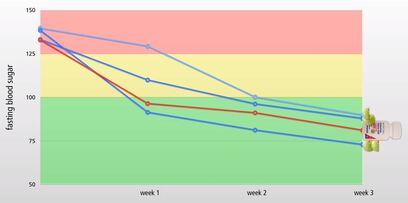
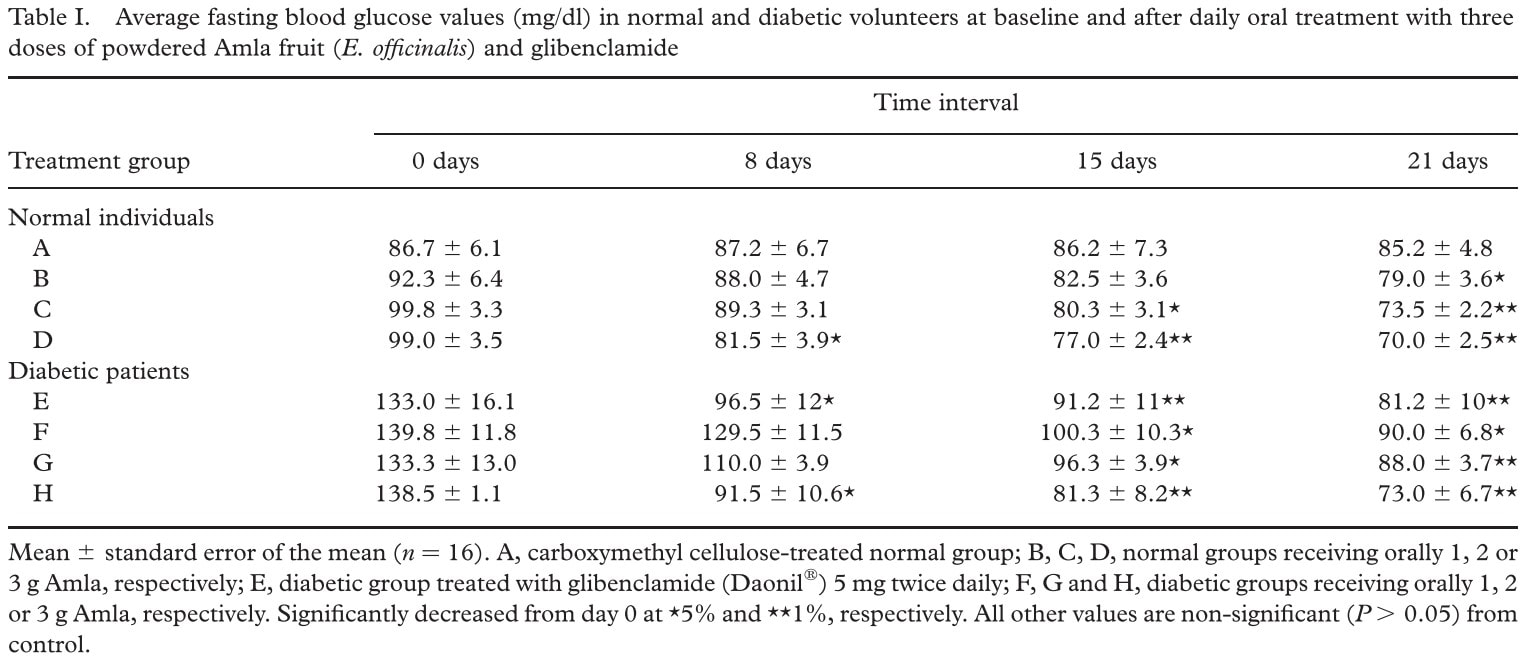
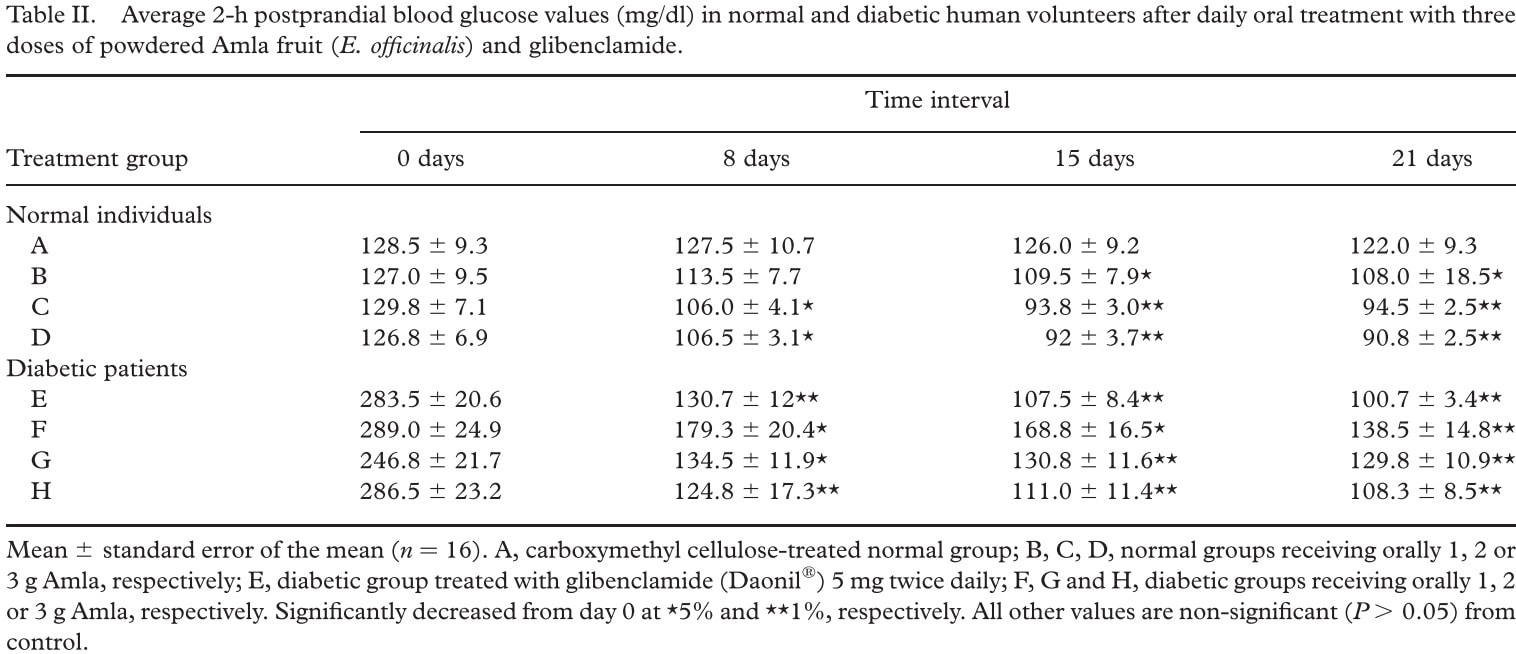
 Image from Neutritionfacts.org Amla vs Diabetes Image from Neutritionfacts.org Amla vs Diabetes Fasting blood glucose (FBG) and 2 hours post meal glucose are two tools used to monitor diabetes and treatment. These tools do not tell the entire story. However, they provide valuable insight and are easy to monitor and track overtime. A small study in Pakistan compared amla powder (Indian gooseberry) to glibenclamide (glyburide). This medication belongs to a class of drugs known as sulfonylureas. One of its many functions is to stimulate the pancreas to secrete more insulin. Amla is a tart fruit used in food and as a medicine in Ayurvedic medicine. Over the last few years, several clinical trials conducted in India and Pakistan show promising result for several conditions. These include hyperlipidemia, GERD, and diabetes. The diabetic group used glibenclamide (a sulfonylurea medication) as a control. Carboxymethyl cellulose fiber served as the control for the non-diabetic group. The intervention groups received 1, 2, or 3 grams of Amla powder (Emblica officinalis) for 21 days. The researchers report a statistically significant drop in fasting blood glucose (see table 1). All the Amla groups showed significant results. Patients given 3 grams had the most dramatic improvement. They started with an average FBG of 138.5 mg/dl.. On day 21 of the study, this group’s average FBG was 73.0. The results for blood glucose 2 hours post meal (postprandial) are also impressive. All doses of amla power showed a significant decrease in blood glucose (see table 2). What are the side-effects of amla?
This same study found that amla power also lowered LDL (the “bad” cholesterol), lowered triglycerides, and raised HDL (the “good” cholesterol). What could be better? Other studies report positive preliminary results for amla as a treatment for GERD, osteoarthritis, and vertigo. However, these studies are preliminary and there is not enough data. [Warning: Do not stop or change your medication without consulting your doctor!] Even with the absence of adverse reaction in the current published literature, there is a potential for interaction with medications. For example, amla can reduce platelet aggregation. This sounds good. However, theoretically, if combined with medications with similar functions, the risk of bleeding increases. Low blood sugar (hypoglycemia) is possible when combined with medications that lower blood sugar. This is theoretical and has not been reported in human trials. Sulfonylurea medications come with their own risks. This medication forces your pancreas to secrete insulin even if you do not ingest carbohydrates. This can result in sever hypoglycemia is you do not eat enough calories and carbohydrates. Another unwanted effect is weight gain. Bottom Line: Should I take amla? Consult with your doctor! I am not saying that because doctors need more patient visits. Ingesting amla in amounts greater than that consumed as food has potential risks. These risks increase when combined with medication. Research into the medical use of amla is still ongoing. It has not been tested for long-term efficacy and safety at high doses. I use amla, in the context of a holistic treatment plan, with some patients. It is not right for everyone. In the end, amla does not defeat diabetes. For some people, it may form part of a good treatment plan. Our goal at Revive Family Medicine is to help you defeat diabetes and regain your health. A transformation of how we live our lives is at the heart of gaining victory and regaining our health. Amla is not the answer. An herb, or any medication, by itself cannot defeat diabetes. Indian gooseberry is an herbal medication that has several plant chemicals. There is an increasing amount of evidence that these chemicals help our body deal with blood sugar, cholesterol, and fat in a way that appears beneficial. References:
2 Comments
 Preparing to write this blog post, I looked for pictures that represented the modern visit to a doctor’s office. Almost every picture I found depicted a doctor facing the patient and hand-writing notes. Has this been your experience? It has not been mine. The media likes to talk about a “healthcare” crisis. This often references limited access to, and the cost of, our medical system. Access to medical services is one issue many people face in today’s medical system. However, perhaps a greater problem we face is the focus of our system. I hesitate to call our system a healthcare system. We focus most of our resources managing disease. I am using these two terms in the following way:
Much of what happens today falls into the disease management category. This is understandable considering that doctors on average only spend 17.6 minutes on each patient visit. During those 17 minutes doctors on average address 6 complaints. Ten minutes to address the primary concern; and 7 minutes to address the other 5 concerns. Most doctors see 20 or more patients every day. That comes out to at least three patients every hour. They spend over 2 additional hours outside of seeing patients in front of a computer completing administrative tasks. Has it ever felt like your doctor spent most of the time focused on a computer screen? If this is your experience, you are not alone. Much of this 17 minutes doctors look at a computer screen, typing, and checking boxes in their electronic health record (EHR) system. This is not an indictment of doctors trapped in this system. Most doctors I know are unhappy with these circumstances. Doctor burnout is high. This is easy to understand when you consider all that doctors face. They are frustrated with documentation demands, lack of quality time with patients, the constant threat of litigation, increased administrative tasks, bloated notes to satisfy insurance (including government insurance), and decreasing compensation. On top of all of this, it is not uncommon for a primary care doctor to have over 2,000 patients on their panel (list of patients under their care). It is understandable that many doctors, either conscious or unconscious, throw up their hand and surrender to the system. How does Direct Primary Care (DPC) help address this problem? In a direct care model of medicine, you have a direct relationship with your doctor. You and your doctor form a partnership centered on the maintenance and restoration of your health. How can this be? In the DPC model, your doctor has fewer patients. Fewer patients leaves more time for each appointment (if needed). This provides the opportunity to treat you as a whole person. The focus can move from management of a disease toward the possibility of the restoration of health. At most DPC clinics, including Revive Family Medicine, you have direct access to your doctor when you need him. For a small monthly fee, about the same as a cellphone plan, you have unlimited appointments, 24/7 electronic access for urgent questions, discounts on laboratory and other services, same day/next day appointments, and so much more. Check out our membership page for more details: ReviveFamilyMedicine.com/membership.html. There are many choices for care. If you want a doctor that will partner with you on your health journey, then DPC may be a good choice for you and your family. DPC provides an opportunity to form a partnership to restore and maximize your health. This is a great choice for those wishing to maintain and maximize their health! It is also a great choice for those dealing with chronic conditions. For more information check out ReviveFamilyMedicine.com/membership.html or contact us to schedule a free 30 minute Discovery session to explore if what we offer is a good fit for your needs. References: Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42(5):1871-1894. doi:10.1111/j.1475-6773.2006.00689.x "Do you spend more time on administrative tasks than your peers?" https://www.ama-assn.org/practice-management/sustainability/do-you-spend-more-time-administrative-tasks-your-peers  In part 1 we consider food. Today we look at movement. I didn’t use the “E” word. As that word sometimes triggers our internal censor; and may get me banned from your feed. 😊 Eksr$ize (one of my more creative spelling moments) is beyond important. Yet, I find this the most difficult aspect of keeping myself healthy. Some benefits of moderate intense movement are: a positive impact on our immune system, resulting in an increase number of white blood cells (our defense force). It also can help us reduce stress and get better sleep—both of which help the immune system. Those who love this look at the rest of us bewildered why we don’t want to spend three hours with them in a stinky gym. I will tell you why I don’t what to do that. First, it stinks. Second, it hurts (and not so good). Third, I do not have a physique to show off. And the list could go on. Now, where should we start? By talking with your doctor to see what intensity is right for you. With that settled, walking for exercise (on top of your daily activities) is a great place to start. We need to answer the questions: How often? How intense? How long? How often? At least three days per week. Five, six, (or even seven) is better. Population studies bear this out. How intense? “Moderate” This is usually described as an intensity where you can still talk, but you could not sustain singing. Start slow. Work your way up to this intensity. If walking is not your thing, then any moderate intensity will do. I start with walking because it is something most people can do without breaking the bank. How long? How much time is also important. The official U.S. physical activity guidelines recommend adults det at least 150 minutes/week of moderate intensity exercise. Even as little as 60 min/week can cause a decrease of overall mortality by 3% (compared to someone more sedentary). 30 minutes 5 days/week (150 minutes/week) provides better results. This may reduce your overall mortality rate by 7%. More is better! Walking twice that (60 min/week 5 days/week or 300 min/week) drops overall mortality by 14%! A study found that 90 minutes of brisk walking (about 4 miles/hour–that is very brisk) was even better. I need to get back to doing this before jumping into a complex program. We cannot buy our way out of inactivity. We can only work our way out. Start small. But start! Work your way up to 150 or 300 minutes per week at increasing intensity. More complex active, if they are of a sustained moderate intensity, work too. Walking is the most accessible. Walk with a friend (but keep up the pace). Walk alone listening to music or a podcast (like Defeating Diabetes is Dr. Dave). Just get out and get moving! But, don't look at your phone-really. [Check with your qualified healthcare professional to insure you are ready to increase your exercise activity. (See, I know how to spell exercise—with the help of spellchecker.)]  Berries are a good source of antioxidants. Berries are a good source of antioxidants. The short, simple answer is YES! Doctors offer throw around advice such as: “Eat better”, “Get some exercise”, “Decrease your stress level”, “Get adequate sleep”. All of this is good advice! In defense of my colleagues, they do not have the time (and sometimes the training or knowledge) to address these complex issues. As a Direct Primary Care physician, I set aside the time to address these needs. As a Naturopathic physician I am trained to deal with the complexities of health, nutrition, disease, and conventional medicine. In this post we will lay the foundation for “Eating Better”. I will cover the other topics in the next few posts. What foods might me most beneficial FOR ME? How do I implement this in my life? Food and nutrition impacts our bodies’ response to infection. It also impacts the chronic diseases we face. Many of these conditions, such as diabetes and heart disease, predict a worse outcome for a COVID-19 infection. What we eat becomes us. Yes, we are rebuilding our bodies all the time. What we eat and drink provide the building blocks. There are some well-established dietary principles. Eating whole, unrefined/processed food diet is a great place to start. Even this can be difficult to figure out. Foods that are high in antioxidants help reduce inflammation, cleanup excessive dangerous “free radicals”, and provide substances our immune system can use to do its job. Vegetables and fruit are high in antioxidants. Meat, dairy, sugar, and process foods are high in substances that promote inflammation. [I know, nobody likes to hear this—me included.] For example, arachidonic acid (a kind of Omega-6 fatty acid) largely promotes inflammation. Red meats are high in arachidonic acid. Omega-6 fatty acids have been linked to elevated blood pressure, blood clots, and increase pain related to inflammation. We need some Omega-6 fatty acids in our diet. Most of us already get way to much! [NOTE: This is for general information only! There are many conditions that require special consideration. Check with your healthcare provider before making significant changes to your diet.] The USDA recommends 5-7 servings of a combination of fruits and vegetables. This is a good general recommendation. Check with your healthcare provider to see if that is right for you. Some (many) of my patients/clients require more. And some (very few) require less—due to specific medical conditions. An array of colors is a good place to start. I only mention two powerful groups below; but there is so much more. The dark blue in blueberries and blackberries (and other berries) are loaded with a powerful group of antioxidants called anthocyanins. Consider including 1-2 servings every day [1-2 cups]. Choose either fresh or frozen. Cruciferous vegetables are rich in substances that support immune function (and a lot of other good stuff). Examples include: broccoli, cauliflower, cabbage, and kale. Consider including 1-2 servings per day. (Check out Eatright.org for serving sizes suggestions). There is so much more to this vast topic. Many need more than a diet plan. They may need a therapeutic nutrition plan. I needed one after my heart attack. Unfortunately, the medical community provided little help in resolving my underlying health issues. This help propel me to go to medical school to learn both conventional standards of care plus nutrition and Naturopathic medicine. It's difficult to cut back on these foods. They have addictive qualities. These foods surround us on every side!. Not to mention, “everybody is doing it.” 😊 I know I need support in this area of my life. I am blessed that my wife and I are on the same page when it comes to food; and to have graduated from a medical program that emphasized therapeutic nutrition. [You may notice I did not mention supplements or herbs. Both can play a therapeutic role. However, it should be based on a foundation of solid nutrition.] I encourage you to find a doctor trained in applying nutrition to address disease to walk with you on your journey. |
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
April 2024
Categories |
 RSS Feed
RSS Feed